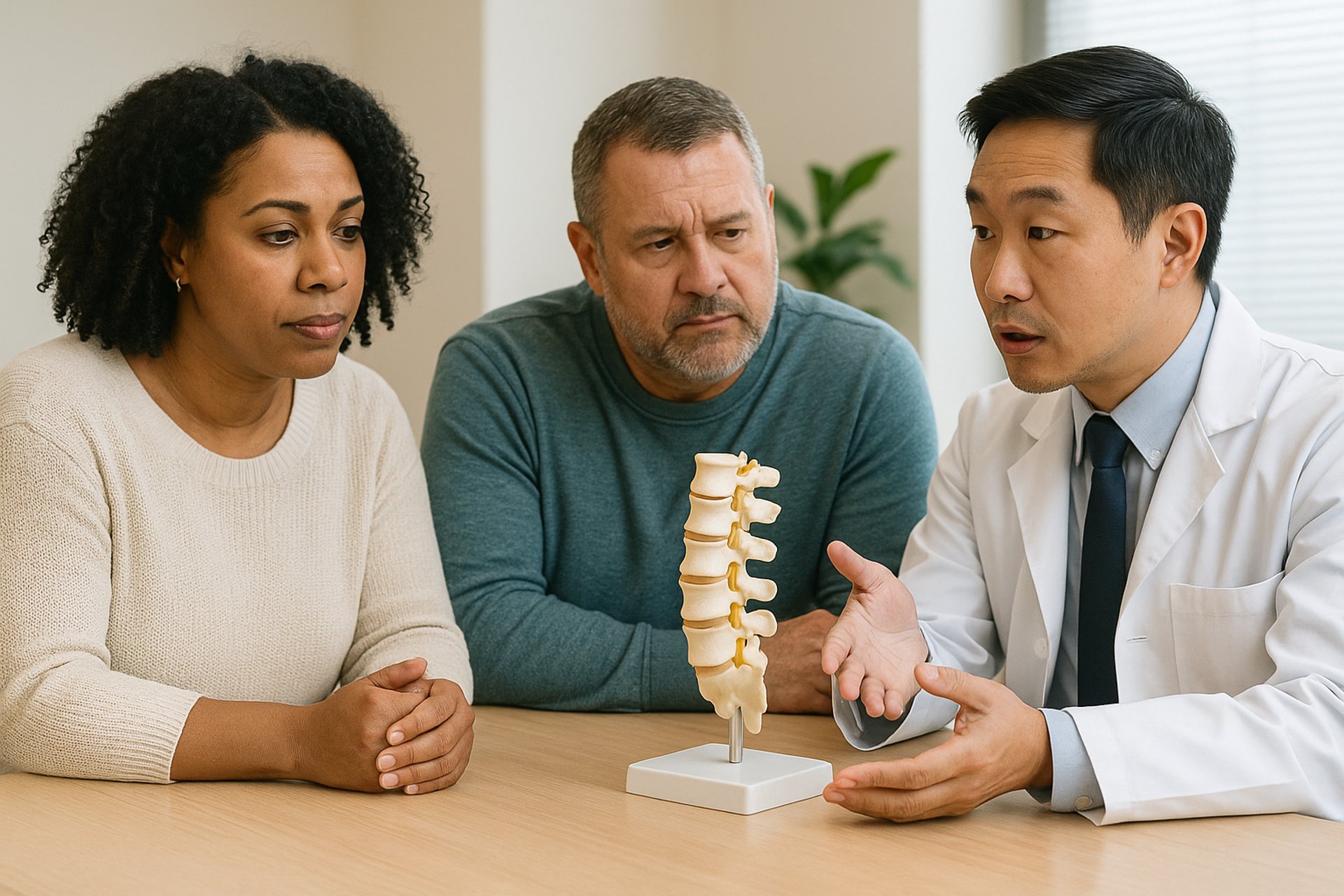
Lumbar Spondylolisthesis
“Spondylolisthesis” (say it with us: spawn-duh-low-lis-THEE-sis) is a condition where one of the bones in your lower back—called a vertebra—slips forward out of place over the one below it.
It most often happens at L4-L5 or L5-S1, the lowest parts of your spine. When the bones move like this, it can narrow the spinal canal or pinch nearby nerves, leading to pain, numbness, and weakness.
There are several types, but the most common is degenerative spondylolisthesis, which develops over time due to wear and tear on the discs, joints, and ligaments that usually hold the spine together.
DSYG You’ve Got Lumbar Spondylolisthesis...
What causes Lumbar Spondylolisthesis?
It’s usually not just one thing. Most people with spondylolisthesis got there from a gradual breakdown of spinal stability.
Common causes include:
Degenerative changes: arthritis and disc wear weaken the joints
Stress fractures (called spondylolysis) that cause slippage
Repetitive strain: years of heavy lifting, twisting, or bad posture (got you sitting up straight now, huh?)
Congenital issues: some people are born with shallow or unstable joints
You might also hear your doctor mention “anterolisthesis” (forward slip) or “retrolisthesis” (backward slip), depending on the direction.
What Can you do about it?
That depends on how bad the slippage is—and whether it’s causing nerve symptoms.
If it's mild and stable, conservative options might help:
Physical therapy to strengthen core and stabilize your spine (really does work but often the most challenging to accomplish)
Activity modification such as sitting up straight or using a standing desk
Bracing in some cases, but usually not an option for adults
Steroid injections for temporary nerve relief
But if you’re experiencing:
Persistent back pain
Leg pain, numbness, or weakness
Difficulty walking or standing upright… then surgery might be recommended.
Lumbar fusion with decompression is the most common surgical approach—often performed as a TLIF (Transforaminal Lumbar Interbody Fusion). This relieves pressure on the nerves and stabilizes the unstable segment.
When Should You Be Concerned?
🚨 Back pain that doesn’t improve with rest or therapy
🚨 Tingling or weakness in your legs
🚨 New trouble standing, walking, or going up stairs
🚨 A visible change in posture—leaning forward or sideways
🚨 Foot drop or changes in bladder/bowel control (urgent)
If your imaging shows a slip greater than 25% or signs of nerve compression, it’s time to talk with your doctor about next steps.